
Today’s New York Times has an article on the sleep problems that lead women to take sleeping pills and attributes the underlying cause to women’s busy lives and childrearing worries. But there was no evidence that the reporter, Pamela Paul, had talked with peri- and post-menopausal women. Single or married they can tell you about the change in the nature and quality of their sleep. And it’s not just women.
I used to be able to sleep anywhere. Now, as a post-menopausal woman, I have nights where I have difficulty falling and staying asleep. But I use to do research on human rhythms and aging, and I know that sleep architecture changes with aging. For example, as we age, the amount of deep sleep and REM (rapid eye movement, or active dreaming stage) declines and sleep becomes more fragmented. So as a nurse, I would ask a patient who appeared to be sleeping soundly during the night (snoring and all) how their night had been. The answer often was, “I didn’t sleep at all.” As a young nurse, I would roll my eyes because I didn’t understand how this could be so. I later learned that if we don’t get that deep and REM sleep, we feel as though we were half-conscious while sleeping.
The ads for sleeping pills play into a myth that our sleep patterns should not change. Consider the home page of the official web site for Lunesta:
“When you want to sleep, do you lie awake? When you get to sleep, do you wake up often during the night? Sleep is here on the wings of LUNESTA. Some sleep aids are approved to help you fall asleep and others to help you stay asleep. Prescription LUNESTA is approved to do both.”
We expect to sleep like a baby when we’re middle and older adults. Maybe we need to reframe how we think about “a good night’s sleep.”
One older woman in a study I conducted 15 years ago told me that when she couldn’t sleep, she just got up and cleaned or read or otherwise occupied her time until she felt sleepy enough to go to bed again. She wasn’t bothered by it. She had reframed what she expected “good sleep” to be. But she didn’t have a job that she had to go to. What makes it most difficult to adapt to changes in our sleep architecture is a sleepless night that’s followed by a full day of work–repeatedly.
I admit to having a supply of sleeping pills that I use mostly for dealing with jet lag from international travel. But I have used them on occasion to ensure I get uninterrupted sleep after nights of sleeplessness and a busy schedule in front of me. How often? Maybe once every three or four months. When I see my nurse practitioner, I ask for only 10 pills, limiting my temptation to think about taking them more often. They are seductive. Those 10 usually last me for a year. I actually look forward to the day when I can get up in the middle of a sleepless night and stay up as long as I want reading a book or writing or cooking.
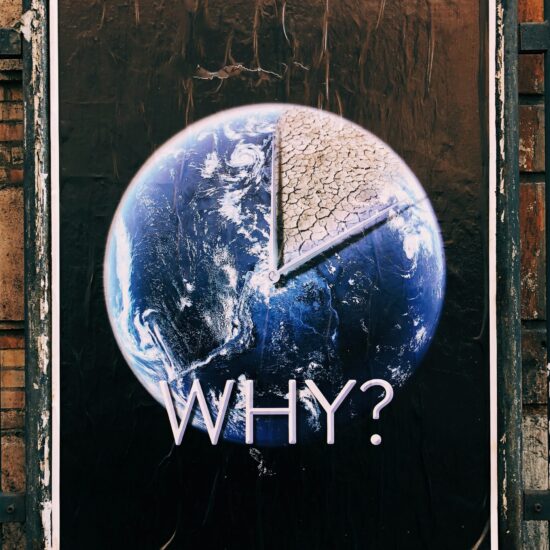
We’re taking botox in our middle years, Viagra when sexual capacity doesn’t measure up to our teenage years, and sleeping pills to sleep like a baby. Our fear and lack of acceptance of aging is stunning. The media messages–whether from ads for “lifestyle” drugs or suddenly-younger-looking TV personalities who are losing their facial expressions from too much botox–are working.
Diana J. Mason, PhD, RN, FAAN, Rudin Professor of Nursing and Co-Director, CHMP







Susan Brindisi / November 6, 2011
All so true.
A secret cure for the sleepless night – do a 12 hour staff nurse shift. Works like a charm….
/
Pingback: Sleeplessness is Only a Dream « Firepitboss / November 16, 2011
/
Pingback: Sleepless in Torbay « newfoundlandtraveller / February 19, 2012
/