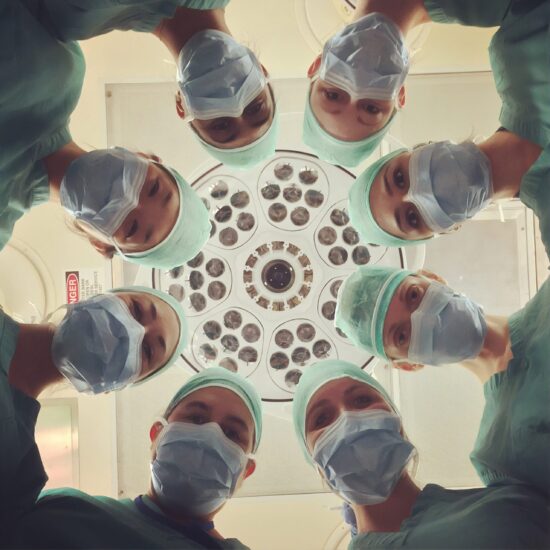
Most would argue that much of today’s rampant costs are associated with a lack of a holistic, integrated approach. This brings up another pertinent topic: our challenge with effective collaborative care.
In our current fee-for-service system, we are often disincented to work in teams. John Weeks discussed the parallel movement to team-based care and the importance of interprofessional education as well as the recent formation of the American Interprofessional Health Collaborative (2011). Backed by Obama’s HRSA, RW Johnson and recent IOM reports, this marks a “historic declaration of core competencies.”
I’m honestly surprised that the push for this has taken so long, considering the IOM’s To Err is Human report from twelve years ago (2000). Having recently graduated from NYU’s nursing school last year, I was horrified to learn how poor quality, bad communication and interdisciplinary disrespect accounted for most lethal medical errors. And despite the integration of healthy collaborative teams in our curiculums, we tend to get a vastly different picture in the clinical setting.
Dean Ornish recounted that it took him 16 years to get Medicare to cover his multidisciplinary model, which includes exercise, yoga, nurse-led support groups, meditation, and nutrition. This allows him to divide payment amongst these individuals efficiently. He stressed that this kind of model is sustainable and allows us to “practice good medicine.”
Nurses are in a prime position to provide individualized attention, as Barbara Dossey, Susan Luck, and Bonney Gulino Schaub, explained in their session on the role of Nurse Coaches. Founders of the Integrative Nurse Coach Certificate Program, they highlight how this kind of therapeutic presence supports the personal transformation that is at the root of change.
Mary Beth Augustine’s talk on Culinary Nutrition described how her multi-faceted approach to working with patients bridges the gap between diagnosis/dietary recommendations and the realities of putting this into practice.
With her partner, she not only gives hands on cooking instruction, but also does personalized needs assessments – including kitchen and pantry makeovers and live grocery shopping lessons. Working in partnership with other providers, this kind of individualized education can be a critical missing link to effective disease management.
While I was a student, I initiated a volunteer program with the NYC Free Clinic, which had been run exclusively by NYU med students for years. And while my initial goal was to gain more clinical experience, I felt that the main value of the program was to provide a hands-on collaborative experience – and what better way to do it than with med students and nursing students within the same university. Needless to say, after months of meetings, emails etc, it became clear that the lack of partnership between our medical and nursing schools was a beautiful example of a much larger problem.
Regardless of this initiative’s inclusion of integrative/CAM practitioners, optimal patient-centered care demands cooperation between all disciplines.