
When I was the editor-in-chief of the American Journal of Nursing, we had a column on pain management that was coordinated by Chris Pasero, RN, MSN, FAAN, a passionate expert on the topic. Pasero and her mentor, Margo McCaffery, PhD, RN, FAAN, had taken it upon themselves to be leaders in educating nurses on how to better evaluate and manage the pain of patients with acute and chronic health problems. They knew of the research showing that too many patients were needlessly suffering with moderate to severe pain because physicians underprescribed pain medication and nurses too often delivered these medications in dosages and with a frequency less than prescribed. In response to this research, leaders in pain management advocated for pain to become the “fifth vital sign” —something that clinicians were to assess regularly (along with the other vital signs of temperature, pulse, respirations, and blood pressure), usually with a 10-point scale on which the patient rated their pain from none to extreme. “Believe the patient’s report” became the mantra for improving pain management.
On several occasions, the editorial staff had conversations with Pasero about the need to address opioid addiction. She would not do so because she feared that nurses would again withhold pain medication from patients out of oftentimes unfounded fears of addiction. It was an understandable argument in an earlier time.
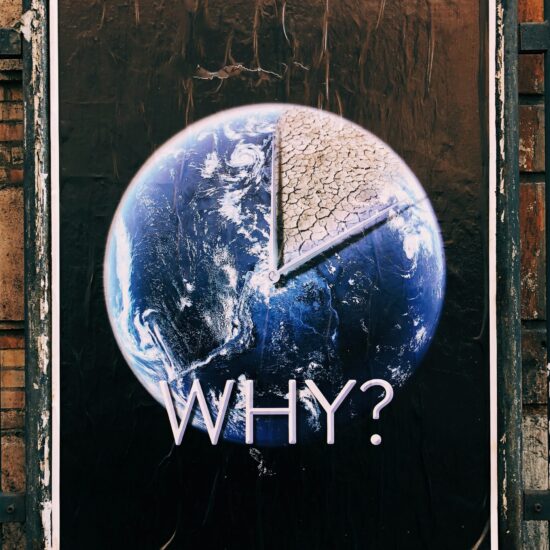
But a recent commentary in JAMA (Journal of the American Medical Association) points out that we must pay attention to the potential for opioid addiction and abuse. Noting that deaths from drug overdoses now surpass those from motor vehicle accidents, Alexander, Kruszewski and Webster challenge us to recognize that opioid abuse is a major public health problem. They point out that the pharmaceutical company may be a co-conspirator in the development of campaigns to eliminate or reduce pain at all costs, since it has resulted in skyrocketing sales and profits for them.
The authors discuss the problem of opioid diversion that occurs all along the pathway from production to dispensing and ingesting of opioids. Most opioid abusers report that they got their drugs through the legitimate prescriptions of family members and friends. I was surprised by the authors’ claim that there is relatively little research that compares the efficacy of various opioids with their adverse effects and abuse.
A few years after my last conversation with Chris Pasero, I interviewed another nurse who works with a peer support system for nurses who have surrendered their licenses while in treatment for licit and illicit drug problems. She argued that we are now too quick to eliminate all pain, all of the time. She asserted that no patient gets addicted to opioids if they are not exposed to it and pushed for scaling back the agressiveness of our pain management approaches. She wasn’t advocating that patients suffer with severe pain or that pain management not be a priority for those who are terminally illl and seek to die comfortably. Rather, she argued for a reasoned, balanced approach to pain management that considers the potential for addiction. So do Alexander and his colleagues.
If I’m in severe pain, I want to be able to request that the pain be relieved and to have clinicians who are sensitive and responsive to this request. If I’m terminally ill, I want to die comfortably and don’t want any clinicians withholding opioids because they fear I’ll become addicted. But what about the potential diversion of these medications by others? That’s a more difficult problem to tackle, but I would argue that a public education campaign may be in order, as well as a national database on opioid prescribing that clinicians can access anytime to determine whether a patient has been over-prescribed these medications.
I was once hit by a car while walking and ended up in Bellevue Hospital’s emergency room. I was in severe pain. I had never had morphine before and, when the nurse gave it to me intravenously, I thought, “Ahh. So that’s what it’s all about.” I then vomited, which I hate to do, and decided that the trip was not worth the side effect. But I understood the attraction of these drugs–their power and their danger. I wonder if Rush Limbaugh understood these things. Does he now? Do others who think they’ll try the opioid high?
Diana J. Mason, PhD, RN, FAAN, Rudin Professor of Nursing







joyjacobson / November 26, 2012
Diana, thanks for a great post, especially for sharing your personal story of severe pain. I also appreciate your writing about how the perspective is shifting in nursing. I wrote a news article for AJN’s September issue — http://bit.ly/PGC1xo — that deals with the question of whether opioids are ever appropriate for chronic noncancer pain. The issue of conflict of interest is huge. “When you’re on the payroll for an industry, it’s very clear that it’s very hard to bite the hands that feed you,” Jeanne Lenzer, a health care journalist, said to me. But a nurse I interviewed saw the ties between researchers and pharmaceutical companies as essential to drug development. I think you’re right that the solution will have to involve intensive education — of clinicians as well as the public. Thanks again.
/
Pingback: THE DOCTOR THAT PUSHED ADDICTIVE DRUGS : Dr. Pinna / December 17, 2012
/
Pingback: Fibro CONTROVERSY « fibromodem / December 23, 2012
/