This post is by CHMP senior fellows Jim Stubenrauch and Joy Jacobson, co-founders of the program in Narrative Writing for Health Care Professionals. Follow them on Twitter: @jimstuben and @joyjaco. 
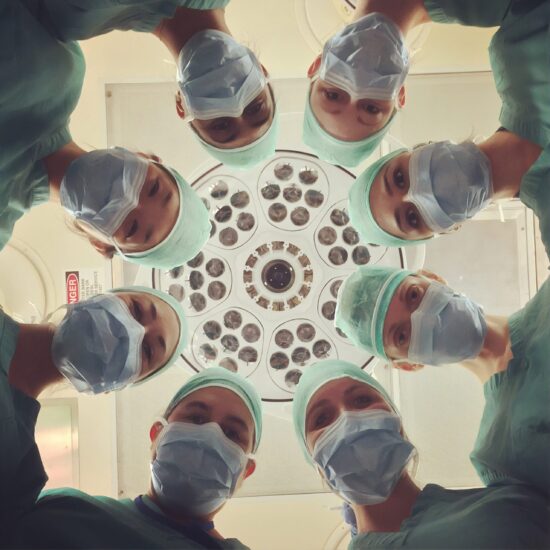
When talking about the work we do here at the CHMP, bringing workshops and classes in writing reflective narratives to nurses and nursing students, we occasionally get puzzled looks. Why teach writing to nurses?
A recent essay in the Narrative Matters section of the journal Health Affairs exemplifies the power of nurses’ narratives and the way personal stories can illuminate larger policy issues.
In “A Nurse Learns Firsthand That You May Fend for Yourself After a Hospital Stay,” Beth Ann Swan tells of a dire medical ordeal: while in Chicago on a business trip, her husband was hospitalized after a brain stem stroke. “In an instant,” Swan writes,
we were thrown into the unreal world of medical “care coordination” and “transition management.” There would be no easy way for us to get Eric from a hospital there to a hospital here and then to home. And along the way there would be gaps in the care Eric received—gaps so large they were more like chasms. We just didn’t know it yet.
It fell to Swan, dean and professor at the Jefferson School of Nursing at Thomas Jefferson University in Philadelphia, to coordinate all aspects of her husband’s recovery, including his transfer from Chicago to a rehab facility in Philadelphia. Even with all of her nursing knowledge and medical contacts, Swan found the following year of coordinating Eric’s outpatient care nearly all-consuming.
In addition to telling this compelling personal story, Swan goes on to advocate one of the strategies for health care reform supported by the Affordable Care Act. Often overlooked in political debates and mainstream media coverage, the ACA’s transitional care initiatives offer real hope of improving health care by bridging the many gaps in our fragmented health care system.
Nurses play a crucial role in transitional care. Swan writes that her husband’s hospital nurses answered questions at any time but that after Eric’s discharge—when they needed as much help as they did during his hospitalization—the nurses were nowhere to be found:
As a patient’s wife, I would have welcomed having an RN as a point of contact. As a nursing school dean, I know the evidence demonstrating that registered nurses are critical to the operational and financial success of health care delivery systems. . . . I also know that nurses have the expertise to bridge care transitions and are critical to coordinating care across all settings.
Swan shows how a well-told story can bring home, with urgent poignancy, a complex topic like transitional care and explain why it should be part of the ACA. (For more on the ACA’s support of new transitional care models, see CHMP co-director Diana Mason’s recent HealthCetera blog post.)
Fitzhugh Mullan, a physician who founded the Narrative Matters column in Health Affairs, said in an interview published in the Permanente Journal that he defined the policy narrative as “an essay form that falls between the editorial and the short story or memoir.” He goes on to say,
It calls for the use of the artful or the insightful in a human and personal way, but with a point, so that the reader leaves not just with an engaging story, but with a kind of an “aha moment” based on what happened to Dr Jones or Miss Smith—we really ought to have better gun laws or antismoking rules or better coverage for children.
As writing instructors at the Hunter-Bellevue School of Nursing, we’ve found our nursing students are eager to craft their personal and clinical experience into poems, blog posts, and narrative essays. It can be thrilling to witness their transformation, as they begin to understand the power of their own stories when told in “artful” and “insightful” ways. In workshops with hospital nurses, too, we’ve seen that writing about the problem solving and bridge building they do every day enables them to recognize—again, often for the first time—the extent to which their jobs consist of advocacy on behalf of patients and families, an insight that renews their sense of the importance of their work.
And who knows how many lives a writer might touch? Theresa Brown, a nurse and a CHMP National Advisory Council member, caught the attention of President Obama with a blog post she wrote about a patient when the president was making the case for the ACA. Stories may not be persuasive in the same way that data and cost–benefit analyses can be. But stories can make the implications of policy proposals understandable in a way statistics can’t. And who would know better than a nurse how to illustrate the importance of transitional care with a personal story?






Pingback: The Most Trusted Profession | Emerging Nurse Leader / December 20, 2012
/