What Would #ThisNurse Say? #NYT, We Are Not Just, “Some Nurses.”
This post is by CHMP’s graduate fellow, Amanda Anderson, RN. Amanda is a practicing bedside nurse in Manhattan, and a grad student at the Hunter-Bellevue School of Nursing, where she co-directs The Nurses Writing Project. Her personal site, This Nurse Wonders, hosts all of her writing, and she tweets @12hourRN.

I gotta say it: I really didn’t want to write about Ebola again. I really did search for an alternative topic, but it’s clear from the media frenzy of the past week’s events – an infected doctor gallivanting around New York City, followed by an Ebola-free nurse-turned political prisoner – that nursing voice on this topic is still direly needed, and still sadly missing.
While nurse-centric reporting has picked up in other media outlets, the Times has largely stuck to its age-old beat – nurses are nameless, unauthorized to speak, and not worth quoting. Perhaps the piece that makes this most evident this week, is Anemona Hartocollis and Nate Schweber’s account of the stigma that the employee’s of New York City’s Bellevue Hospital face while currently treating Ebola. Honestly, after “Bellevue Employees Face Ebola at Work, and Stigma of It Everywhere,” I’ve toyed with the idea of cancelling my subscription and switching to the Post, because it really doesn’t read much different.
I’m sad, and a little flabbergasted by this piece. It speaks of stigmas Bellevue workers are facing since Ebola came to town – an important topic, and a perfect opportunity for nurse input. While I am sure that the burden of high profile care for Dr. Spencer and a condition as dangerous and unfamiliar as Ebola, is stressful and emotionally taxing, this article does little to break down the stigma that it speaks of. In contrast to Emory Health’s full disclosure of care protocols, this is wasteful public relations fluff. Where expert nurse opinion may have offered salve to the burns of misinformation, this collection of random quotes from titled physicians and food cart workers instead fanned its flame.
While any number of nurses could have commented in a way that discredited the reported stigma, not one was named or quoted. Instead of an infection control nurse talking about the procedures employees follow when entering and exiting the hospital (do they shower after work at Bellevue, as they do at Emory?), or the Chief Nursing Officer speaking about the counseling and supportive practices given to nurses caring for patients, nurses were referred to en masse as, “some nurses,” or “workers.” Instead of a union steward discussing the bargaining that is likely taking place to ensure that Bellevue nurses are adequately trained and units safely staffed throughout the care of this patient, nurses filed rank with the unskilled, unnamed and unauthorized – silently embracing the stigma, perhaps.
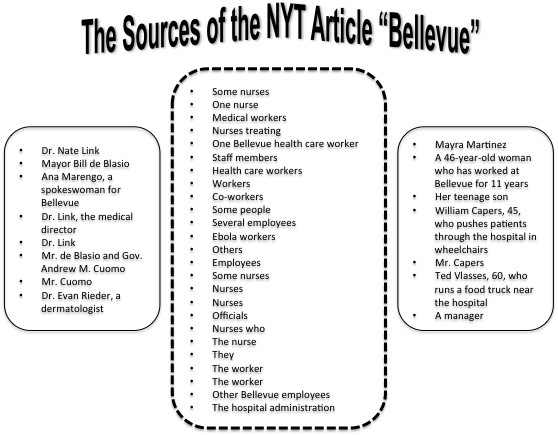
Sources, as listed by NYT reporters Anemona Harticollis and Nate Schweber, in their article, “Bellevue Employees Face Ebola At Work, and Stigma of It Everywhere,” from October 29, 2014.
The message behind this article is clear, through the language of speech that surrounds each person interviewed – nurses are not important enough to be identified, to be trained to speak openly to the media, or to be titled. While the man who sells coffee on the street shares his name and opinion, the expert, educated nurses within the hospital are shushed. Perhaps the contrast between those allowed to speak and those quoted in anonymity exposes a larger truth: Unless we are at a staged press conference, or whistle blowing with a lawyer, nurses are to remain the quiet ghosts of healthcare.
What would this nurse say, as my pithy title so blaringly asks? I’d say, nurses, start asking why the authors of an article in The New York Times can get away with quoting and titling the man who pushes patients down the hall, but you, the educated, credentialed professional are not sought after. I’d say, prepare yourself to speak to these reporters; start by reading your employer’s media policy, and asking your public relations department for nurse-specific media training. Remind them of your worth as an expert whose voice of experience is vital in current conversation. Tell them that with one sentence, a well-spoken nurse might have changed the course of this article from tabloid fodder, to a positive and effective public information piece: Ebola care is challenging, but because we are trained in x, y, z, and because we want to see our patient, and our community remain healthy, we push through with vigilance and skill.
Without our names, our titles or our words, we will continue as, “…some nurses,” allowing those without our expertise to speak for us, and own our care.
This post is by CHMP’s graduate fellow,







