According to the Advisory Board, almost 50% of those eligible to enroll for health insurance under the Affordable Care Act this year are between 18 to 34 years old. This makes the launch of Open Enrollment 3.0 particularly important to my friends, who text me all the time with their health questions: “Hey, I chopped the tip of my finger off while cooking tonight. Should I go to the ER? Here’s a photo,” is not a strange message to receive when you’re a nurse.
Obamacare turned five this year, and open enrollment season, which launched November 1st, turned three. The system has come a long way from its infancy, with healthcare.gov preparing for a whopping possible 10.4 million eligible enrollees for this 2016 season.
Enrollment, it seems, is just the first step in creating healthy Americans – many of my friends are covered, thanks to the Affordable Care Act, but they don’t know how to use their coverage, or where to get help when they need it. Health care delivery, or how we get to the providers that facilitate our newly prized coverage, is what my friends are most concerned about.
Heath economist and physician-writer, Aaron Carroll, summed up our current healthcare delivery reality in his description of the arduous process that he undertakes four times a year in order to obtain medication for a chronic condition:
“The Affordable Care Act, which seems so complicated to so many, was almost entirely about getting more people in the United States health insurance. That was just a first step, arguably an easy one, and we’re still fighting about it. Reforming the ways in which we actually deliver care and try to improve outcomes? That’s so much more important, and we barely talk about that at all. But that’s what matters to the people who use the system, and it’s why so many of them are frustrated.”
What an incredible statement, considering Carroll’s vast experience with the system as a physician. How do less knowledgeable patients fare?
This makes the work of the non-profit The Young Invincibles (YI), especially important. YI is an organization that works to give young people – millennials, specifically – a voice in areas like political advocacy and health. Over e-mail, I interviewed the new YI Northeast division director, Kevin Stump, about his position, YI, their health initiatives, and their new app, HealthYI, which launched this fall.
Kevin Stump, Northeast Director for the organization, Young Invincibles.
I downloaded HealthYI to my iPhone recently. Along with my surprise at how fast it launched (woo-hoo to a low-tech app that doesn’t suck my battery dry), I found that I really liked the program’s simple, ALL CAPS html-ish layout: HEALTH CHECKLIST tops a bold list of four selection options, including MONEY-SAVING TIPS. Fitting, since Federal officials have expressed concern that cost is a reason for Healthcare.gov 3.0 being “tougher” for new-enrollees than in prior years.
Although each option leads to some pretty text-heavy pages, HealthYI has some great, basic content for new patients. As a nurse who has treated urban patients of all ages since before the first iPhone was created, I’ll certainly use this at work and with friends looking for a primer on health insurance. The content is welcome; Americans, especially young ones, really don’t know how to be patients, simply because they haven’t had coverage for so long.
The HEALTH RIGHTS menu of HealthYI is remarkably comprehensive, with sections pertaining to immigrant rights and LGBT, too. While the SCHEDULE AN ANNUAL PHYSICAL choice doesn’t include my health plan, it looks like a great start, and its platform, which zips through selections without a cinch, will likely appeal to data-restricted young folks looking for a quick and easy guide to understanding health insurance for the first time. Overall, the app is a definitive resource for pointing young people toward the information they need to gain health literacy in an unobtrusive, easily maneuvered way.
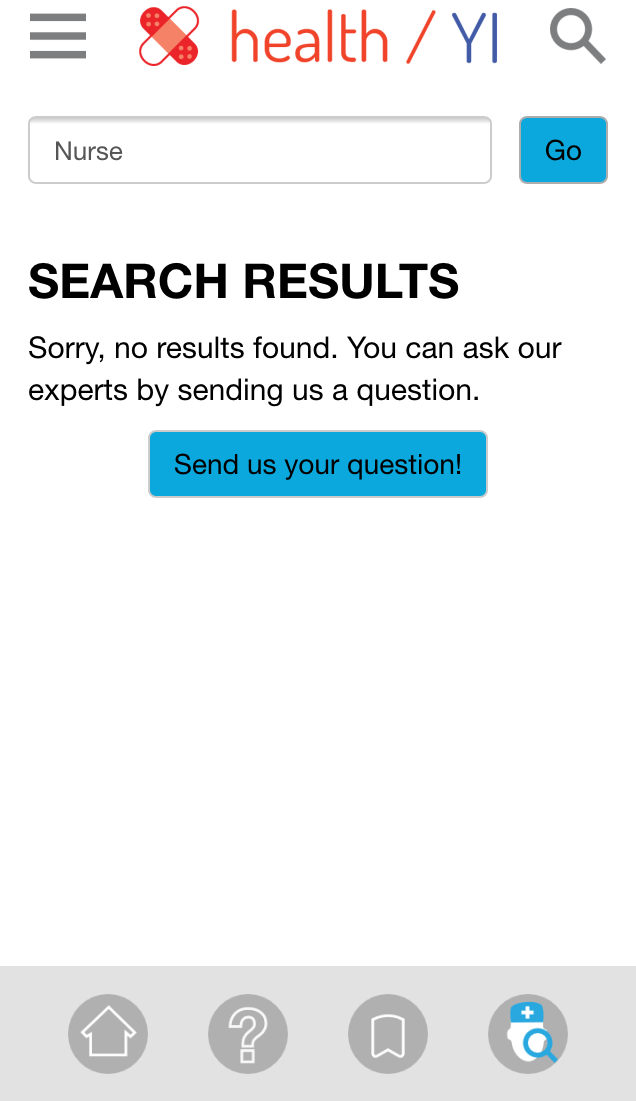
What stumped me, though, and will perhaps serve as a plausible impetus for launching a league of talented tech-savvy nurse YI volunteers, is the “SEND US YOUR QUESTION!” section. While YI promises to respond within two business days, it doesn’t capitalize on what all insurance companies already provide, and what my texting friends so frequently have no clue about – the oft-overlooked number on the back of every insurance card that leads directly to the 24/7 service of a preventative, available, expert nurse.
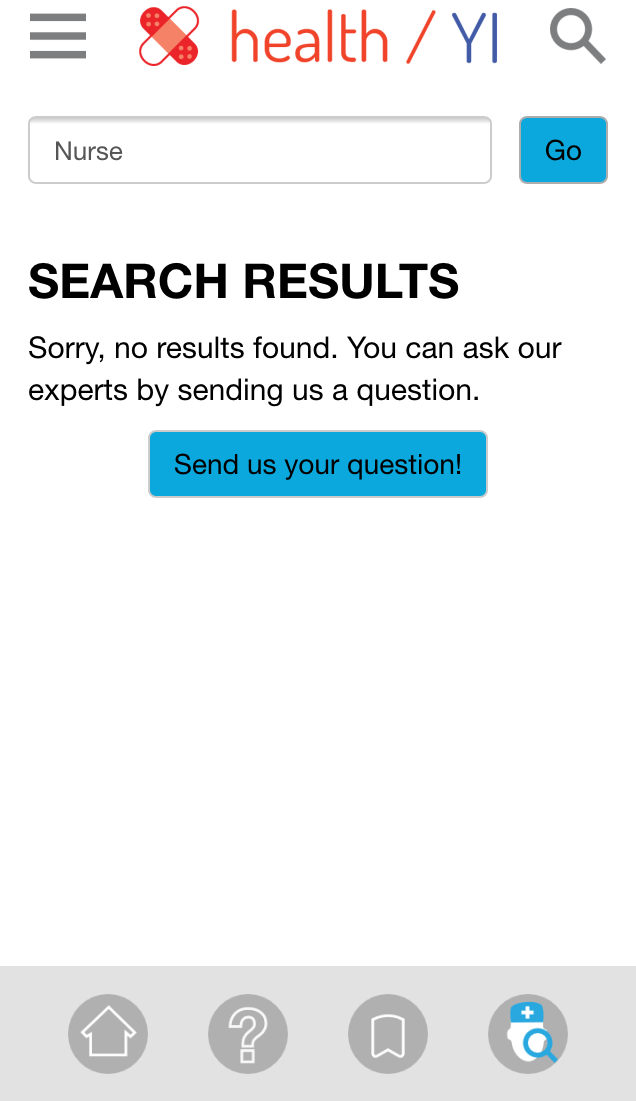
Results of a search in the HealthYI app.
I was especially puzzled when my query for “nurse” in the search function of HealthYI came back totally empty – nurses might connect, educate on, and speak to all of the possible selections this tool has to offer – from finding providers to answering money-saving questions. In other words, would my friends stop texting me, if apps like this hooked them up with a live nurse instead?
Here are some October 2015 excerpts from my exchanges with Kevin, Northeast Director of Young Invincibles, who tweets @KevinStump:
Why YI? What, specifically, about the organization interested you?
Young Invincibles fills a much needed gap in advocating for and elevating the voices of Millennials, a generation that has too often been left out of today’s most critical policy and societal debates.
Millennials were hit the hardest by the Great Recession, and so many hardworking young adults are still facing the ripple effects. Today Millennials still face unique challenges in simply trying to gain an economic foothold – an unemployment rate that is nearly 40 percent higher than the national average, skyrocketing college costs resulting in crippling student debt, and a lack of awareness around affordable healthcare options and how how to use them.
In New York and across the country we are tackling these issues and beyond through research, policy, advocacy, organizing, and more. Our perspective must be heard wherever decisions about our collective futures are being made.
Tell me about this new YI app — What about it do you think works really well? Doesn’t?
The HealthYI app was designed by YI Advisors, Young Invincibles’ non-profit consulting arm, with a number of New York regional partners to bring healthcare to the fingertips of young New Yorkers.
This is especially relevant today because young adults are increasingly accessing services via their smartphones. The app not only provides basic and easy-to-understand resources like a health checklist, tips on how to save money, health care rights and insurance basics, it allows users to schedule an appointment with a healthcare provider or send in a personal question and get an answer.
We’re also collecting feedback and watching how young adults use it, as we want to make sure we’re continually adapting and improving the app based on the real needs of its users, so there will likely be more updates and potential new features to come.
What’s your plan for getting YI into the hands of those it hopes to serve – young people? What barriers do you face – nationally, but regionally, too?
We’re working hard to get the word out there about the new app, with a special focus on reaching typically underserved and low-income communities, which historically have less experience with healthcare options.
We are continuing to build new partnerships, for example we’re working with the CUNY University Student Senate and School of Public Affairs to connect this tool to their students. Additionally, we are reaching Millennials where they consume information — on their mobile devices — through a paid social media campaign targeting New York City residents.
And we’re already hearing some great results – for example we heard from one young woman who lives in New York City and used the app to find a sports medicine physician after tearing a muscle. She has put it off for the past month because her health care provider’s website is so difficult to navigate. In less than 10 minutes, she downloaded HealthYI and was able to schedule an appointment.
A lot of studies are showing that young people, tech savvy ones, even, would rather pay the tax penalty than enroll in insurance because delivery is so poor. Seeing any glimmers of hope on the horizons, or any programs that YI is excited by/pairing with?
We know that young adults want and value coverage, and now that affordable options are available to them, they are signing up. In New York State, 34 percent of those who enrolled in health coverage during the last open enrollment were Millennials, age 18-34.
According to the Advisory Board, almost 50% of