Source: National Academies of Science, Engineering and Medicine
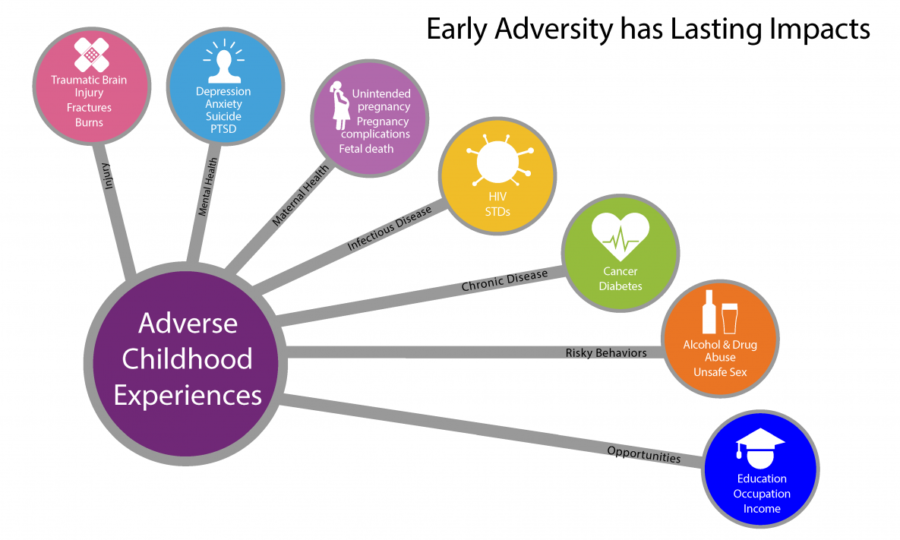
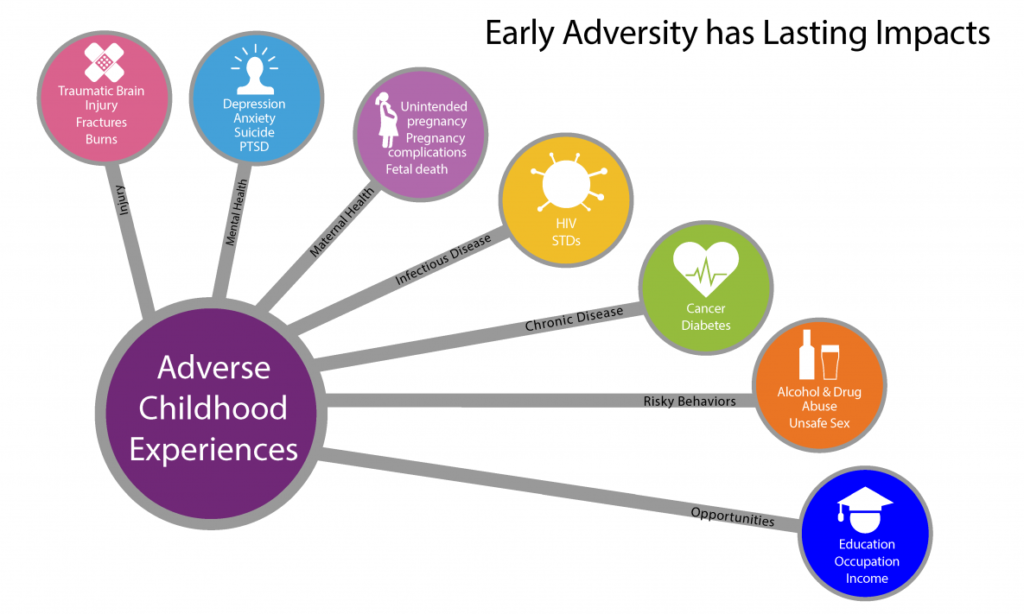
Evidence is mounting that social determinants of health affect both health outcomes and costs. Health can be powerfully influenced by things like access to nutritious foods, adequate housing, education, violence, environmental contaminants and other conditions where people live, work and play. Someone’s recovery from an illness can be profoundly affected by these determinants. Consider the person with diabetes who is discharged on insulin and a special diet. If that person is homeless, the insulin can’t be refrigerated, and adhering to a special diet may be impossible.
Too often, the health care delivery system ignores these determinants. But this is beginning to change as evidence mounts that failure to address these determinants, even at the individual level, will result in poor outcomes and higher costs. When health care organizations and providers participate in global, value-based payment approaches, it’s in their best financial interests to address patients’ social needs, as well as to advocate for policies and population-level strategies to improve the health of whole communities. Such strategies can include advocating for low income housing or community gardens or job training programs.
The National Academies of Science, Engineering and Medicine recently released a new report titled, Integrating Social Care into the Delivery of Health Care. This is only one in a series of reports addressing social determinants of health and social needs care that NASEM has published in recent years. As health systems experiment with how to better address their patients’ social needs, the new report provides evidence-based recommendations. I was pleased to serve on the committee that prepared the report, along with Robyn Golden, MS, LCSW, Professor in the College of Health Sciences at Rush University and Associate Vice President of Population Health and Aging at the University’s medical center. She also directs Rush’s Center for Health and Social Integration. Robyn and I talked about the report on HealthCetera in the Catskills on the day of the report’s release, September 25, 2019. You can listen to it here:
HealthCetera in the Catskills with Robyn Golden
Podcast: Play in new window | Download
Subscribe: Email |
[caption id="attachment_14915" align="alignleft" width="200"] Source: National Academies
 Today, there are over 5.3 million people in the United States 65 years of age or older who are living with dementia and that number is estimated to triple by 2050. It’s also the 6th leading cause of death among older adults. Valerie Gruss, PhD, RN, Clinical Associate Professor of Nursing and Director of ENGAGE-IL (Enhancement of Geriatric Care for All) at the University of Illinois at Chicago, has been identified as an “Edge Runner” by the American Academy of Nursing for her work to help people with dementia and their families learn how to best manage the illness. She developed the Dementia Guide Expert App that provides information on dementia, its symptoms, how to diagnose it, treatment options, and, most importantly, how to manage the disease. The app includes links to other resources and services for both the person and their family caregivers.
Today, there are over 5.3 million people in the United States 65 years of age or older who are living with dementia and that number is estimated to triple by 2050. It’s also the 6th leading cause of death among older adults. Valerie Gruss, PhD, RN, Clinical Associate Professor of Nursing and Director of ENGAGE-IL (Enhancement of Geriatric Care for All) at the University of Illinois at Chicago, has been identified as an “Edge Runner” by the American Academy of Nursing for her work to help people with dementia and their families learn how to best manage the illness. She developed the Dementia Guide Expert App that provides information on dementia, its symptoms, how to diagnose it, treatment options, and, most importantly, how to manage the disease. The app includes links to other resources and services for both the person and their family caregivers.