Social networking & crisis support: Facebook’s new anti-suicide tool
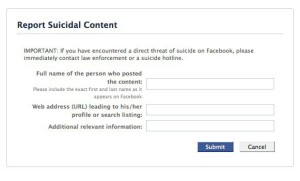 On Tuesday, December 13, Facebook, in collaboration with the Substance Abuse and Mental Health Services Administration and the National Suicide Prevention Lifeline, launched a new anti-suicidal tool that allows users in Canada and the United States to report potentially suicidal postings they see on the site. Once the user highlights the content, the person who posted it will receive an email with a toll-free number to speak directly to a counselor or to click on a direct link to a private, online chat session with a counselor from the National Suicide Prevention Lifeline.
On Tuesday, December 13, Facebook, in collaboration with the Substance Abuse and Mental Health Services Administration and the National Suicide Prevention Lifeline, launched a new anti-suicidal tool that allows users in Canada and the United States to report potentially suicidal postings they see on the site. Once the user highlights the content, the person who posted it will receive an email with a toll-free number to speak directly to a counselor or to click on a direct link to a private, online chat session with a counselor from the National Suicide Prevention Lifeline.
Surgeon General Regina M. Benjamin commended Facebook and Lifeline for addressing suicide — which she described as one of America’s most tragic public health problems. In a statement she said that nearly 100 Americans die by suicide every day.
“We have effective treatments to help suicidal individuals regain hope and a desire to live and we know how powerful personal connections and support can be,” she said. “Therefore we as a nation must do everything we can to reach out and provide them with the help and hope needed to survive and return to productive lives with their family, friends and communities.”
This new Facebook tool appears to be the first active effort by a social media site to identify people in the midst of a mental-health crisis and get them directly to a health professional.
Science writer, Nancy Shute, blogged for NPR’s health blog, Shots, on this new anti-suicide tool and raised the issue of privacy and HIPPA regulations. She also wonders what’s next for Facebook users – “Before too long, hearty eaters could perhaps start getting referrals to Weight Watchers, or the American Diabetes Association.”
Barbara Glickstein, RN, MPH, MS co-director CHMP
On Tuesday, December 13, Facebook, in collaboration



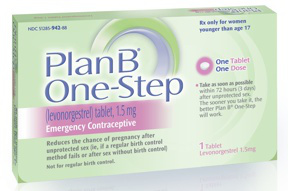
 Currently, no one under 17 can buy the Plan B pill from a pharmacist without a prescription; young women must show proof of age. The FDA seemed about
Currently, no one under 17 can buy the Plan B pill from a pharmacist without a prescription; young women must show proof of age. The FDA seemed about 
